Smarter Claims Processing for Faster Cash Flow
This blog is part of an ongoing series exploring how Aera Skills solve real-world supply chain challenges.
Efficient claims management is critical for maintaining healthy cash flow and strong customer relationships — yet achieving it consistently can be a challenge. That’s where AI and automation can help, providing the intelligence needed to accelerate resolution, reduce manual work, and improve settlement accuracy.
With the Claims Management Skill, the Aera decision intelligence agent has achieved claim coverage exceeding 90 percent, reduced manual effort by more than 80 percent, and improved resolution accuracy to above 85 percent. These results enable finance and customer service teams to resolve claims faster, operate more efficiently, and strengthen customer satisfaction.
The Challenges: Manual Work, Data Complexity, and Inconsistent Resolution
Many organizations still rely on manual work and disconnected systems to process customer claims. These inefficiencies slow the billing-to-cash cycle, create errors, and overburden specialists. Common challenges include:
- Manual claim processing requiring extensive review, categorization, and resolution by claim specialists.
- Complex data management where claims must be matched against sales orders, billing documents, and contract terms.
- Inconsistent claim handling due to claims arriving in structured formats (spreadsheets) and unstructured formats (PDFs, emails).
- Resource-intensive workflows requiring integration across claims systems, sales orders, master data, and communication channels.
Left unresolved, these issues create billing delays, hinder cash flow, and strain customer relationships.
The Aera Solution: AI-Driven Claims Management
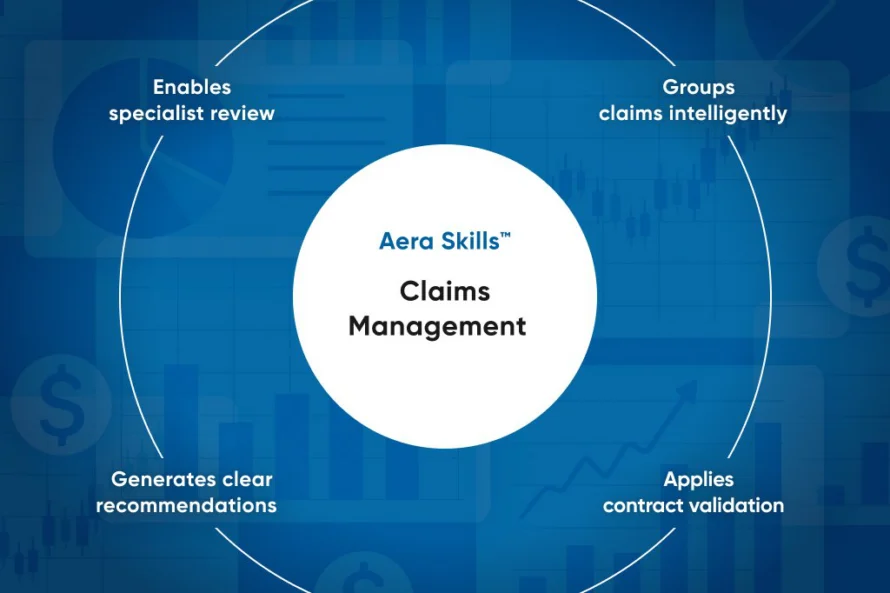
Aera, the decision intelligence agent, uses the Claims Management Skill to automate claim validation and processing from end to end. This transforms claims management into a faster, more accurate, and scalable system of action by:
- Grouping claims intelligently by type, amount, and data availability across structured and unstructured sources.
- Applying contract validation against contracts, pricing agreements, promotional terms, and master data to calculate accurate settlements.
- Generating clear recommendations to confirm valid claims for settlement or notify customers of invalid claims.
- Enabling specialist review by integrating recommendations into workflows, allowing experts to focus on approvals instead of research.
Behind the scenes, Aera applies a team of AI agents that structure data, validate it against contracts, and apply reasoning logic to assess legitimacy. Document processing, contract matching, and decision rules combine to deliver reliable, automated claim outcomes.
Case Study: From Bottlenecks to Accelerated Resolution
A leading consumer packaged goods (CPG) company faced delays and inconsistencies in claim resolution that slowed cash flow and overburdened specialists. Manual reviews across multiple contract types and agreements created bottlenecks and frequent errors.
After deploying Aera with the Claims Management Skill, the company automated claim categorization, contract validation, and recommendation generation. Within just a few months, it achieved:
- >90% coverage of claims
- >80% reduction in manual effort
- >85% accuracy in claim resolution
These improvements accelerated resolution times, reduced operational workload, and improved customer satisfaction.
Why Aera: What Sets It Apart
Aera transforms claims processing from a manual, error-prone task into a streamlined, intelligent process powered by AI and automation. It replaces complexity and inconsistency with speed, accuracy, and consistency, so teams can focus on making better decisions, not managing claims data.
- Unified decision intelligence: Aera integrates claim data, contract validation, and settlement logic into a single solution.
- AI-augmented workflows: It improves claims efficiency by applying composite AI and intelligent automation across the full claims lifecycle.
- Closed-loop execution: Valid claims are automatically processed and invalid claims trigger clear customer notifications, accelerating and standardizing resolution at scale.
With Aera, finance and customer service teams can move beyond slow, manual processes and toward faster, more reliable decision-making — confident that their claims are accurate, timely, and actionable.
Ready to transform your claims management?
For more on how Aera can help you achieve faster resolutions, eliminate manual effort, and improve accuracy, download the Claims Management Skill brief or schedule a demo.







